Research Spotlight

Building Better Biologists:
A New Program Trains the Next Generation of Science Educators
The University of Georgia (UGA) is home to a large and robust group of biology education researchers (BER). Collectively, this group has a long and strong record of training postdoctoral fellows who go on to pursue a variety of careers, including research and teaching intensive positions in higher education, positions in faculty professional development, and others. One of the reasons for the success is the diverse and collaborative environment in the social and behavioral sciences. Many faculty at UGA with research programs in biology education have ongoing collaborations with faculty in educational psychology, psychology, science education, higher education, and other disciplines.
A team co-led by Dr. Erin Dolan, an OIBR distinguished scholar, Georgia Athletic Association Professor of Innovative Science Education, and professor of biochemistry and molecular biology, and Dr. Logan Fiorella, also an OIBR distinguished scholar and associate professor of educational psychology, is fostering a new generation of BER through an exciting initiative funded by the National Science Foundation (NSF).
This project, titled “Preparing the Next Generation of Biology Education Researchers through Interdisciplinary Co-mentorship and Evidence-based Professional Development,” tackles a crucial challenge in the field of BER. Traditionally, BER research has been criticized for being isolated from other disciplines, limiting its impact, and hindering the development of robust theories on teaching and learning biology.
“Given the rich scholarly and training environment at UGA, and our collective networks and collaborations, we thought we could put together and facilitate a rigorous and supportive postdoctoral training program that was focused on cross-disciplinary research in biology education,” said Dr. Dolan.
She explains, “Imagine studying how students make decisions about careers in the life sciences or how students learn to solve life science problems without considering the science of motivation or problem-solving. That’s the kind of isolation we’re aiming to bridge.”
This new program directly addresses this issue. Biology education research investigates teaching and learning in life science fields by combining the priorities, worldviews, knowledge, and practices of biology with the research methods, tools, approaches, and theory from the social sciences. By leveraging UGA’s wealth of BER faculty and experts in social and behavioral sciences, the project will train postdoctoral fellows in a truly interdisciplinary environment.
Why is this important?
BER plays a vital role in improving how biology is taught and learned. It investigates how students develop as life scientists and come to understand life science concepts and their applications and implications. But without a strong foundation in other disciplines like psychology and education, BER research can struggle to build a comprehensive picture.
This research project aims to change that. Postdocs in the program will be co-mentored by BER faculty and researchers from other relevant fields. This unique approach will equip them with the tools and perspectives to conduct more impactful and theoretically grounded BER research.
Collaboration is Key
Dr. Dolan highlights a particularly rewarding aspect of the project: the collaborative spirit among faculty. “It has been such a pleasure to work with the faculty involved in the project,” she says. “Everyone is coming to the project with an open mind, generative spirit, and collegial ethos.”
This collaboration extends beyond the faculty. The project prioritizes equity and inclusion in its recruitment process. Potential applicants can participate in virtual office hours and submit “curiosity statements” instead of traditional research statements. This approach focuses on aligning applicants’ interests with the program’s goals, fostering a diverse and dynamic learning environment for the incoming postdocs. Dr. Dolan stated, “Applicants are responding very favorably to these elements,” pointing out “that it is one of the reasons they were attracted to apply to the program.”
The Road Ahead
The project is funded for three years, with postdocs receiving two-year appointments. While future funding from the NSF is uncertain, the potential for expansion is exciting. Dr. Dolan envisions recruiting additional cohorts in the coming years, allowing the program to continue its mission of building a new generation of well-rounded BER researchers.
This initiative promises to revolutionize BER by fostering a collaborative and interdisciplinary approach. By training the next generation of researchers to think outside the box, the program paves the way for a brighter future in biology education, ultimately benefiting students and the field.
More info.: Erin Dolan
Written by: Andrea Horsman

SPRING 2023
RESEARCH SPOTLIGHT
Dr. Sun Joo (Grace) Ahn
Associate Professor, Advertising & Public Relations
Dr. Sun Joo (Grace) Ahn never thought she would become an academic. Her dad worked in sales for a very long time at multinational corporations in South Korea, and Grace still remembers her dad telling her about the challenges of leading large, integrative teams of people from different backgrounds and the excitement of finally being able to close a deal after months of preparation. She said, “I didn’t really understand much of the content of what was being said- but was always in awe of how the adult world worked and at the multinational scale of things.”
Looking back now, though, Grace shared that “it’s funny how my dad’s experiences and wisdom delivered to me during long conversations over dinner impacted my career choices: I love thinking about how persuasive messages can be designed and evaluated, the processes and outcomes of persuasion, pulling together large integrative teams for research, and ultimately developing interventions for large-scale attitude and behavior change. I never intended to be a professor of advertising but maybe my dad secretly knew all along!”
“Studying persuasion is a constant lesson in humility and the appreciation of diversity,” said Dr. Ahn. “Communication science is complicated and fascinating, because it is very much a relational science, where interactions between the medium, user, and contextual details all matter. The human stands at the center of our science and their lived experiences play a key role in how persuasive messages are processed and interpreted. Understanding the diversity and complexity of these relationships and designing a successful intervention to modify behavior, particularly in the context of everchanging technologies always keeps me on my toes,” Grace said. “What surprises me most about working on these types of projects is that understanding human behaviors and how they interact with technologies never, ever gets any easier (despite all these years)!”
Communication undergirds almost every human activity we can think of; it’s omnipresent. As a result, there are many more armchair scientists in this neck of the woods than there may be in, say, physics or chemistry. Grace added, “It’s surprisingly challenging to get noncommunication scholars to understand what communication science is and why it is important. Despite the seemingly frivolous nature of our research topics (e.g., entertainment, video games, social media), we employ systematic and rigorous methodologies to address our scientific inquiries.”
“Media and communication are weaved into almost every part of our lives and we are far more impacted by mediated communication than we realize; yet, it’s often a challenge to be taken seriously when your area of research is virtual reality, avatars, and video games.”
Grace has over 20 years of training and experience in media psychology with an emphasis on technology-integrated community-level interventions. She is currently serving as the Deputy Director and a MPI of the Center for Children’s Health Assessment, Research Translation, and Combating Environmental Racism, which is part of her current $4.5 million grant from the National Institute of Environmental Health.
The Center for Children’s Health Assessment, Research Translation, and Combating Environmental Racism (CHARTER), works to develop effective strategies to translate research findings of importance to children’s environmental health to relevant stakeholders in the community, academia, and healthcare. The research team with CHARTER know that working with community partners are the key to developing communication products that can be used to improve children’s health. The center acknowledges the structural nature of health inequity and is working on projects that address how structural inequities can negatively impact children’s health via research projects and community engagement (e.g., social media activities, training community health workers, K-12 outreach programs).
In recent years, Dr. Ahn has really expanded her partnerships with grassroots, non-profit organizations in the community, translating science into actionable, technology-mediated interventions. “When I launch interventions with these community partners, my research team gets to know them well and over the years, and we develop strong friendships with people who share our vision of leveraging science to help people live happier, healthier lives,” she said. “Being able to directly see and interact with community members and observe the positive impact of my research really makes all the hard work worth it. As many of us understand, this job is much more than “just a job”—it creates a lot of meaning in my life. The thrill of making discoveries and generating new knowledge never gets old, but I truly love the opportunity to be able to give back to community through my research. I think that intrinsic reward is what keeps me up working late at nights and drives a lot of the motivation behind my recent work.”
“My research program that started out with a small $20,000 internal grant has now become a sizeable enterprise with over $10 million in extramural funding. The interesting thing is that none of these people are in the field of communication; but their mentorship, guidance, and friendship over the years has allowed my scholarship to dramatically expand beyond its initial narrow focus to something that is much more transdisciplinary and meaningful,” Grace added.
More information about Dr. Ahn’s research: Center for Advanced Computer-Human Ecosystems (CACHE)
More info.: Grace Ahn
Written by: Andrea Horsman

FALL 2022
RESEARCH SPOTLIGHT
Dr. Cynthia Suveg, Ph.D.
Professor, Psychology
GRANT TITLE:
A culturally informed model linking physiological stress regulation and behavioral and academic adjustment in Latinx children
FUNDING SOURCE:
National Institutes of Health
AWARD & AMOUNT:
R01 for $3,117,133.
GRANT TIMELINE:
8/1/2022 – 7/21/2027
CO-INVESTIGATORS:
Margaret Caughy, Professor, HDFS
Justin Lavner, Associate Professor, Psychology
Interviewed by Andrea Horsman
Approximately a decade ago, Dr. Cindy Suveg received pilot grant funds from OIBR as well as funds from a NIDA parent grant housed in the Georgia Center for Contextual Genetics and Prevention Science within the Center for Family Research. At that time, she wanted to learn more about how biological processes interact with environmental factors to influence development, and those pilot grants allowed her to do that and were foundational to the R01 that she was recently awarded.
Building off of her past pilot grant research Dr. Suveg understands the Latinx population in Athens and the surrounding communities is growing, yet Latinx families are underrepresented in research. This is especially problematic because Georgia is a new immigrant area which means that local communities may be less likely to have the infrastructure in place to support Latinx families than communities in states where immigration is more established.
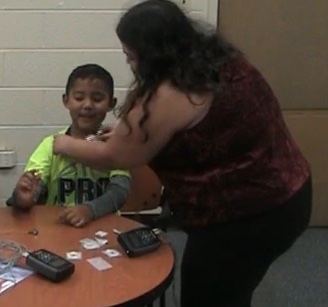
Dr. Suveg and her team are focusing specifically on Latinx families with young children and using a cultural neurobiological approach to identify predictors of school readiness in Latinx children and the ways that parents support healthy development in their children. They will also examine factors that influence Latinx parents’ own well-being.
The study will include assessments of biological, behavioral, and sociocultural environmental factors across individual (child), interpersonal (parent-child relationship), and societal (immigration stress) levels over a 3-year period. The team hopes that study findings will offer novel information about the ways that culture and biological processes intersect to influence the well-being of Latinx families.
Dr. Suveg is grateful for the opportunity to work with very inspiring mentors during her research career. Her graduate school mentor, Dr. Janice Zeman, and postdoc mentor,Dr. Phil Kendall, were genuinely enthusiastic about the research process and were committed to mentoring. She is very thankful to have had these mentors who encouraged her to think deeply about things and enjoy the research process.
Reflecting on her research, Dr. Suveg said, “Hearing directly from families about their experiences is the most rewarding.” “I go into this work with hypotheses about things, but I always learn way more in the process than I knew when I started. This research also requires a very strong team to do it successfully, and I find it rewarding to work with collaborators both here at UGA and beyond, as well as a big team of outstanding students.”
More information about this research: Development & Psychopathology (DAP) Lab

Fall 2021
RESEARCH SPOTLIGHT
Dr. Ewan Cobran Ph.D.
ASSISTANT PROFESSOR, CLINICAL AND ADMINISTRATIVE PHARMACY
Interviewed by Andrea Horsman
Grant Title/Research Project: Genetic Literacy and Patient-Caregiver Communication of Prognostic
Genetic Technology for Localized Prostate Cancer
Funding Source and Amount: National Cancer Institute Mentored Research Scientist Development K01
Award – $862,985.00
Grant Timeline: 09/10/2020 to 08/31/2025
How did you first get involved with this project?
I began studying prostate cancer disparities at Howard University in 2010. After completing graduate school, I completed a Cancer Health Disparities T32 Postdoctoral Fellowship in 2014 at the University of North Carolina at Chapel Hill, Lineberger Comprehensive Cancer Center under the mentorship of Dr. Eugenia Eng and Dr. Paul A. Godley. As a Postdoctoral Fellow, I received a pilot grant award to evaluate racial differences in morbidity, disease control, survival, and use of Intensity-Modulated Radiation Therapy (IMRT), for prostate cancer using the Surveillance, Epidemiologic and End Results (SEER)-Medicare Linked Database. Using data collected during the early years of IMRT diffusion from the SEER-Medicare Linked Claims Database (cohort of 10,975 prostate cancer patients), I found a significant geographic variation in the diffusion of IMRT, including differential use by SEER region, race, urban/rural residence, and residence in areas with varied regional educational attainment. The use of SEER-Medicare Linked Claims Database sparked an interest in precision oncology and genetic literacy. In 2019, with immense support from the Georgia Clinical & Translational Science Alliance, I was awarded a Research Supplements to Promote Diversity in Health-Related Research by the National Center for Advancing Translational Sciences. This project focused on evaluating facilitators and barriers to the comprehension for the application of genomic technology for prognostic testing among rural white and African American men with localized prostate cancer. The specific aims of the project were (1) to develop a genomic literacy education video for the comprehension of common genomic terminology for prognostic genetic testing in patients with localized prostate cancer; and (2) to examine facilitators and barriers to the comprehension for the application of genomic technology for prognostic testing among patients with localized prostate cancer. This project served as the preliminary study for the current funded project.
Tell me about this project and why it is important:
Precision oncology is rapidly expanding, specifically for prostate cancer.
The National Comprehensive Cancer Network (NCCN), in2016, recommends patients and clinicians consider tissue-based genetic tests for localized prostate cancer to help patients make more informed treatment decisions at the time of diagnosis.
Specifically, Oncotype DX, Prolaris, Confirm MDx, Promark, ProMark, and Decipher multi-gene mRNA expression panels offer new approaches for categorizing patients according to their levels of risk for biochemical recurrence or metastasis. With this greater certainty regarding prognosis, men with prostate cancer are now equipped to make more informed decision about the appropriateness of conservative management with active surveillance versus immediate treatment. However, while much enthusiasm currently exists for the burgeoning field of genomic medicine, the use of multi-gene mRNA expression panels raises the potential for further divergence in prostate cancer treatment outcomes by race and low socioeconomic status. We know that health disparities persist in low-income groups despite the existence of evidence-based guidelines and that adoption of state-of-the-art methods often lag behind in these groups. We posit that if common barriers to adoption, such as lack of understanding of genetic testing (e.g., genomic comprehension), low levels of formal education, and lack of knowledge regarding prostate cancer persist, systemic disparities with regard to prostate cancer treatment will be perpetuated even with the availability of good treatment options.
The goals of this project are to (1) explore how men with localized prostate cancer and their caregivers comprehend prognostic genetic technology, and (2) examine how an educational video about genetics impacts patient-caregiver communication of prognostic genetic technology. The study rationale is that without direct attention to genomic comprehension, the enthusiasm that exists in the rapidly increasing field of prostate cancer genomic medicine may not translate into health benefits for men with localized prostate cancer. The central hypotheses are (1) men and caregivers with lower levels of education will demonstrate a severe lack of genomic comprehension of tissue-based genetic tests for localized prostate cancer; and (2) tailored prostate cancer education, communication coaching, and a genomic literacy educational video will significantly improve patient-caregiver communication in underserved population.
Where can people go if they want to learn more?
The National Cancer Institute and the Precision Medicine Initiative
Tell me about someone who has influenced your decision to work in Cancer Disparities:
In 2008, I lost my maternal grandparents to cancer. My grandparents died 5-months apart. Coping with late diagnoses, consecutive deaths, and funerals of my grandparents provoked me to dig into the cyclical process of late diagnosis, lack of prevention, lack of treatment, and lack of support, which results in death for the underserved. After the second funeral, I realized that I wanted my scholarship to actively help eliminate barriers to early cancer diagnosis and prevention.
What do you find most challenging about the research you are doing?
Research can be exhausting, and you often experience lots of failures. There is a certain level of determination, grit, and persistence that is required.
What do you find most rewarding about the research you are doing?
I love community-based participatory research. The impact of community partnerships in helping to shape the direction of the research project is priceless.
What direction would you like to see your research to take in the next five years?
I am planning to conduct a R01 randomized community-based participatory research study, to evaluate prostate cancer patients’ and caregivers use of predictive genetic technology and treatment decision.
Go here for more information about Dr. Cobran’s research.

Spring 2021
RESEARCH SPOTLIGHT
Dr. Kristen Shockley, Associate Professor, Psychology
Interviewed by Andrea Horsman
Owens Institute Distinguished Scholar Dr. Kristen Shockley, PhD, an Associate Professor of Psychology at UGA, was awarded $149k for a rapid response grant from the National Science Foundation for her research entitled, “Collaborative Research: Adjustment and Effectiveness of Rapid Transition to Remote Work.” Grant Timeline- May 15, 2020 – April 31, 2021.
Kristen is a University of Georgia alumni (Psychology, 2004). She received her Ph.D. in Industrial/Organizational Psychology from the University of South Florida in 2010 and she has been a member of the UGA faculty since 2016.
We recently caught up with Kristen and asked her to share some information about her research.
How did you first get involved with this project?
A colleague alerted me of the special call for RAPID grants in response to the pandemic in mid-March 2020 – actually the day that UGA announced it would close for two weeks. I started brainstorming the idea with my Co-PI, Tammy Allen at the University of South Florida, shortly thereafter. We submitted our proposal by the end of March and heard that we were going to be funded 8 days later!
Tell me about this project and why it is important.
The COVID-19 pandemic forced much of the country’s workforce into remote work arrangements. With the need for social distancing, the ability to continue essential business functions through effective remote work arrangements has been a key means for addressing the global health crisis. However, many organizations were unprepared to accommodate a remote workforce and likewise lack insight into best practices as to how to promote continued productivity and well-being of the workforce in such arrangements. Our study was designed to address this need; the overarching goal was to provide evidence-based recommendations to organizations so that they can function optimally in times where remote work is necessary. We did this by obtaining data from an occupationally-diverse set of 498 participants who were not working remotely before the pandemic but had transitioned to full-time remote work as a result. We collected baseline data to get a sense of stable organizational and individual factors and overall adjustment and then asked the participants to respond to a survey every day for four weeks so we could track changes over time and more precisely model how daily experiences impact daily wellbeing and performance.
What has surprised you most about working on this this type of project?
I am continually amazed at the willingness of our participants to provide daily data. It’s a lot to ask. I am also surprised to hear their comments about participating in studies – namely how they value the introspection that it forces in thinking about their day and the way they manage work and family.
What do you find most challenging about this research?
Recruiting participants is often a challenge. Most of my research focuses on work-family issues and necessitates dual-earner couples with children. Those seem to be the busiest people who don’t always have time to participate.
What have you found most rewarding about this research project?
Research finds that managing work and family is a very prominent stressor in our society. Knowing that I can in some way contribute to the knowledge base to help alleviate those struggles is really rewarding.
Tell me about someone who has influenced your decision to work in Psychology.
I completed my undergraduate degree at UGA and was influenced by OIBR’s very own Lillian Eby (Psychology) as well as Janet Frick (Psychology) who taught me Introduction to Psychology as a first semester Freshman.
What is your personal philosophy on what should be done in regards to further advancing your research?
My current philosophy is to try and do research that will have clear applied implications and answers basic questions that we still don’t know the answer to. For instance, people always ask what can they do to facilitate work-life balance, and I think most of the existing research relies on what organizations can do rather than specific strategies individuals can use. I’d like to move more in the direction of doing meaningful research that is also meaningful to people outside of academia.
What direction would you like to see your research take in the next five years?
I think the personal philosophy answer overlaps with this one. But in terms of specifics, I am very interested in studying women’s unique experiences in the workplace that are related to the transition to motherhood, such as fertility and breastfeeding. I am also interested in studying populations that have historically been under-researched, such as military spouses, given the challenges in maintaining a meaningful career due to the demands of military life.
Where can people go if they want to learn more about your research?
We have produced a few different reports from this data which are available on my website: https://iwillugaresearch.wixsite.com/website/publications

SPOTLIGHT: Owens Institute Turns 50
Written by: Andrea Horsman
The Owens Institute for Behavioral Research (OIBR) is celebrating its 50th year of supporting social and behavioral science research at the University of Georgia.
In 1970 the Social Science for Research Institute formally became the Institute for Behavioral Research (IBR) and William A. “Bill” Owens was appointed the founding director. The Institute had goals of fostering interdisciplinary research and enhancing scholarship in the Social and Behavioral Sciences on campus. Owens foresaw the shift from single discipline “method focused” research to interdisciplinary “problem focused” research and he brought social and behavioral scientists together across disciplines to tackle pressing social issues.
In the mid-eighties, the second director of IBR, Abraham Tesser (Psychology), recognized that social science researchers at the university greatly lacked support to seek extramural funding. It was his efforts that created a support system within the institute to develop a greater emphasis on the role of extramural funding in developing and maintaining outstanding scholarship in the Social and Behavioral Sciences.
During this time, the Center for Research on Crime and Delinquency officially became part of IBR. The center name has changed several times over the years, but now it is known as the Center for Research on Behavioral Health and Human Services Delivery. Paul Roman (Sociology) was appointed as director of the center in 1986 and he remains the director 34 years later.
The Center for Family Research (CFR) was established in 1985 with Rex Forehand (Psychology) appointed as the director. Gene Brody (HDFS) was appointed director in 1994 and he still holds the position, with co-director Steve Beach (Psychology). Under Brody’s leadership, CFR activities began to focus more specifically on the reciprocal impact of children, their caregivers, and the broader community context on health and psychological adjustment among African American families living in the rural South. This center remains one of the most successful centers on campus and its research impacts not only families in Georgia, but across the United States.
In 1989, the Junior Faculty Research Mentoring program was created pairing junior faculty with a senior research faculty mentor for twelve months. This program provided grant development support and thirty-one years later the program is still highly successful. The Grantsmanship Development Program has provided grant writing education and support to over 120 social and behavioral faculty members and is a hallmark of the Institute.
Steve Beach was named the fourth director of IBR and he further enhanced the status and visibility of the Institute. In 2011, he was instrumental for the renaming of the Institute in honor of Bill Owens and his wife, Barbara, who continued her husband’s legacy with a $1 million gift that created an endowment for the William A. and Barbara R. Owens Institute for Behavioral Research. The fund is used to foster the kind of collaborative research and faculty mentoring that Bill Owens championed.
Today, as the fifth director, Lillian Eby (Psychology) guides OIBR, we continue to enhance research in the social and behavioral sciences in a number of ways: mentoring junior faculty in grant writing; offering seminars and colloquia from leading social and behavioral scientists from across the globe; assisting departments in their recruitment efforts; and we also continue to offer streamlined comprehensive pre-award and post-award grant support to reduce grant-related administrative burden for investigators.
Currently there are six Centers of Excellence under the institute including Center for Family Research, Center for Gambling Research, Center on Biological Embedding of Social Events and Relationships, Center for Integrative Conservation Research, Center for Research on Behavioral Health and Human Services Delivery and Scientists Engaged in Educational Research (SEER). In addition, there are six thriving work groups that provide multi-disciplinary collaboration opportunities for scientists in a supportive intellectual environment for the pursuit of their research. They include Cognition and Neuroscience group; Computational Social Science work group; Psychological Assessment work group; Relationship Science work group; Stress, Trauma, Adversity & Resilience work group and the Violence work group.
Over 175 social and behavioral scientists are affiliated with the Institute. These scientists, in collaboration with each other and graduate students, are addressing basic and applied cutting edge research questions in the arenas of health, family, education, culture, conservation, and sustainability. These activities and contributions are the result of the hard work of the faculty affiliated with OIBR, sustained support from the Vice President for Research, the cooperation of departments and colleges across campus, and the dedication and hard work of the Institute’s support staff.
The institute has grown exponentially over the last 50 years by consistently reaching a 30% hit rate for funding. The programs nurtured by OIBR not only attract faculty with some of UGA’s largest grant awards at UGA, but also make a positive impact in the lives of many individuals in Georgia and elsewhere.
Fifty years later, we have stayed true to Bill Owens core principles of mentoring, advocacy, collaborative research, and supporting social and behavioral science research. The cornerstones of OIBR include encouraging and supporting innovative research; fostering collaboration across disciplines; mentoring our junior faculty; providing resources to support rigorous scientific research; and inspiring and celebrating the successes of our scientists.
We hope you will join us throughout the next year as we host special events to celebrate our success and look forward to the future!

Spring 2020
RESEARCH SPOTLIGHT
Paula P. Lemons, Professor (Biochemistry and Molecular Biology) & SEER Center Director
Interviewed by Andrea Horsman
Dr. Paula Lemons, PhD, is a Distinguished Scholar of the Owens Institute and Professor of Biochemistry and Molecular Biology. She received her B.S. at Southern Wesleyan University, her Ph.D. in Biochemistry at the University of Kentucky, and completed a postdoctoral fellowship at Duke University.
She has a passion to help students develop a deep understanding of science and the ability to solve real-world problems. During her postdoc years she transitioned to social and behavioral sciences research and became interested in problem solving and assessment. Her career was launched in biology education research, a relatively young interdisciplinary field, in which researchers investigate basic questions about learning, teaching, and the sociocultural context of undergraduate education.
Dr. Lemons is working on several research projects to transform STEM (Science, Technology, Engineering, and Math) education. We caught up with her and asked her to share some information about her STEM research and education at the University of Georgia.
How did you first get involved with STEM?
I received my PhD in biochemistry studying basic biology – how blood platelets secrete clotting factors. As a postdoc I transitioned to social and behavioral sciences research and I immediately became interested in problem solving and assessment. I had a passion to help students develop a deep understanding of science and the ability to solve real-world problems. I knew this focus had been lacking in my own education, and I wanted to make a difference.
During those postdoc years, I connected with colleagues with backgrounds in math and science education. They introduced me to research areas that required expert knowledge of science and social science methodologies, including classroom observations, clinical interviews, and qualitative data analysis. These collaborations launched my career in biology education research, a relatively young interdisciplinary field, in which researchers investigate basic questions about learning, teaching, and the sociocultural context of undergraduate education.
Tell me about your involvement in STEM research.
I teach biochemistry and I am conducting research in biochemistry learning. When I was a junior faculty member teaching biochemistry to sophomores and juniors here at UGA, I speculated that life science undergraduates’ early problem-solving skills may have long-term effects. That is, students who solve problems well as early undergrads experience success and that success feeds back to them in positive ways to propel persistence. In contrast, students who struggle to solve problems as early undergrads experience failures that feed back to discourage persistence. Part of my research is examining this idea – and a number of related ideas – in the context of biochemistry-specific problem solving.
Tell me about one of your research projects and why it is important.
In 2014 I was awarded a $900,000+ grant from National Science Foundation for a six year research project entitled, “Problem Solving Skills as Predictors of Success and Persistence in Biology.” This study aims to describe the biochemistry-specific problem-solving skills of life science students as they progress through their undergraduate course work at the University of Georgia. We have assessed the biochemistry problem-solving skills of hundreds of students in introductory biology, intermediate biochemistry, and advanced cell biology. This spring we will complete data collection for a cohort of 200 students who started their life science courses in fall 2016 or spring 2017. We collected cross-sectional data from hundreds of other students.
Through students’ written solutions and interview responses we have pinpointed challenging aspects of biochemistry problem solving. For example, the diagrams and models used for teaching often confuse students and contain implicit information that students miss. Also, students tend to describe biochemical phenomena superficially unless prompted to describe the underlying processes. Our research shows that explicit instruction can overcome these challenges.
This project also aims to identify the relationships among biochemistry problem-solving performance, affective and demographic variables. This summer, with our longitudinal data collection complete, we will use latent growth modeling to determine the changes in biochemistry-specific problem-solving performance over time for our sample of 200 students. Simultaneously, we will investigate the extent to which students’ self-efficacy and intrinsic motivation predict performance and the extent to which gender, URM status, and SES moderate these effects.
Conducting this research in biochemistry is important because biochemistry is one of the key courses taken by STEM majors, particularly pre-health professionals and biochemical or biomedical engineers. Biochemistry also offers an interesting context because students begin learning the basic concepts as early as high school through introductory biology and general chemistry courses, yet they typically do not deeply integrate their knowledge of biology and chemistry until college biochemistry.
Understanding learning challenges is important because surprisingly little is known about what makes science difficult. For biochemistry, we know it is abstract and that students must learn things they cannot see, but the particular stumbling blocks have not all been studied. Uncovering these challenges in detail provides a road map for improving instruction.
Understanding the relationships among problem solving, affective variables, and demographic variables will reveal how the experiences of different types of students vary and suggest ways to intervene to create sociocultural environments that make success and persistence attainable by all students.
What do you find most challenging about this research project?
The most challenging aspects of this research project have been developing assessments and collecting longitudinal data. We cannot directly measure what students know about biochemistry or their ability to apply their knowledge. Instead we depend on indirect measures – students’ responses to problem sets. We spent years developing assessments that passed the scrutiny of experts and the pilot testing of students. Even though we settled on assessment items that have provided rich and meaningful data, we know different assessments would reveal different aspects of student knowledge.
We have relentlessly worked with the UGA Office of Institutional Research and life science instructors to track and collect data from the students in our longitudinal cohort. We attempted to anticipate all paths and scenarios and to create strong incentives for students to complete all the data collection activities. We are pleased with our success, but it has challenged our wits and our patience.
Tell me about some of the people you’ve met through your research.
This project has opened up exciting collaborations at UGA and beyond. At UGA, I collaborate with Allan Cohen, Hye-Jeong Choi, and Logan Fiorella all in the Department of Educational Psychology. Al, Hye-Jeong and I collaborate on the psychometric analyses of our problem-solving assessments. We also are using the biochemistry problem-solving data to test new methods like topic modeling. Topic modeling is a type of statistical modeling that allows for the discovery of “topics” in a collection of documents. We are looking for topics in student writing that may reveal new patterns in student thinking and problem-solving process.
Logan and I collaborate to understand the impact of evidence-based pedagogy on student learning in biochemistry. Logan brings expertise in investigating general learning mechanisms that may apply across educational contexts, and I bring expertise in the particular challenges of learning biochemistry. Together, we aim to test general learning mechanisms in disciplinary contexts that are persistently troublesome for students.
Outside of UGA, this work has led to an exciting collaboration with cognitive psychologist Mark McDaniel (Washington University) and chemistry education researcher Regina Frey (University of Utah) who are interested in individual differences in students learning tendencies that impact their performance in science courses. Specifically, they have shown that some students tend to learn by focusing on examples, while other students tend to learn by abstracting across examples. This tendency is distinct from intelligence or academic achievement. We will be using the biochemistry problem-solving assessments developed for this project to investigate the importance of individual learning tendencies in biochemistry.
Finally, this work has led to collaboration with Jennifer Loertscher at Seattle University. Jennifer specializes in biochemistry education and related research and led a national coalition to determine the most critical concepts in biochemistry education. Jennifer and I work to apply biochemistry education research to the classroom and assist faculty in using the research.
Tell me a little bit about the DeLTA research project.
I am the Principal Investigator for a $3 million NSF funded project called, “Transforming STEM Education at Research 1 University through Multi-Level Action Teams,” that was awarded in 2018.
This project involves over 100 faculty members in biology, chemistry, engineering, mathematics, physics and statistics working together to explore ways to better support, incentivize and reward effective, evidence-based STEM instruction and are creating, implementing and assessing active learning materials to help students better develop STEM knowledge and skills.
The project is formally known as DeLTA (Department and Leadership Teams for Action), and it is inherently a team effort. My co-principal investigators are Tessa Andrews (Genetics); Peggy Brickman (Plant Biology); and Erin Dolan (Biochemistry and Molecular biology). In addition, Associate Provost for Faculty Affairs Sarah Covert is also a co-principal investigator. We will be working with UGA senior administrators as well as department heads and other collaborators over a five year period on this project.
What do you think/hope will change regarding STEM over the next five years?
In the next five years, I hope more equity will be achieved in STEM education. Currently the majority of students who enter college intending to pursue a degree in STEM leave STEM. This problem disproportionately impacts women, underrepresented minorities, and students from lower socioeconomic status. Discipline-based education research has revealed a number of ways to address this problem. For example, pedagogies that actively engage students in learning can reduce failure and withdraw rates and improve learning gains. We also know that helping students build self-efficacy and science identity can improve their science achievement.
Individual courses and faculty play dramatic roles in maximizing student learning and supporting students to develop the affective characteristics that facilitate their success and persistence in STEM. Yet college faculty do not have training in pedagogy, and research faculty are not typically even evaluated on their teaching. Thus, I also hope that in the next five years, university departments and institutions will act to take undergraduate education more seriously. This will involve a combination of increased support, professional development, and accountability. We need ways to honor the expertise of faculty and help them learn how to roll that expertise into modern teaching approaches that match what we know about student learning.
Where can people go if they want to learn more about your other research?
I lead an interdisciplinary center on campus known as Scientists Engaged in Education Research, or SEER. The SEER Center includes faculty, postdocs, and graduate students across the University of Georgia who perform research in collegiate STEM education. As science and technology continue to expand their relevance for life in the 21st century, and as a scientifically educated workforce is under increasingly short supply, there is a pressing need for solutions to improving science education in the United States, and specifically to transform how science is taught and learned in colleges and universities. Research areas include basic and applied research grounded within STEM disciplines and informed by evidence-based theory in educational and social sciences. Research generated by participants in the Center catalyzes the transformation of STEM teaching and learning locally and nationally.

Fall 2019
RESEARCH SPOTLIGHT
Dr. Jody Clay-Warner (Sociology)
Interviewed by Andrea Horsman
Dr. Jody Clay-Warner is a Meigs Professor of Sociology in the Franklin College of Arts and Sciences and has been at the University of Georgia since 1998. She received her Ph.D. in Sociology from Emory University, where she took comprehensive exams in both Social Psychology and Criminology. She also earned a Certificate in Women’s Studies. Dr. Clay-Warner is the co-director of the Laboratory for the Study of Social Interaction (LASSI) and the co-Director of the Violence Work Group at OIBR. In addition to many UGA committees, she is currently on the editorial board of Emotion Review and is on the Executive Board of the International Society for Research on Emotion, where she serves as treasurer of the Society.
Dr. Clay-Warner has been the recipient of many distinguished awards, including:
- Women’s Leadership Fellow, University of Georgia, 2017-2018
- Owen’s Creative Research Award for Distinguished Contributions to the Behavioral & Social Science, University of Georgia, 2017
- Fellow, Society for Experimental Social Psychology, inducted 2009
- Lifetime Achievement Teaching Award, American Society of Criminology, 2013
She loves to teach and this semester she is teaching a graduate seminar on Theories of Social Psychology. This class is fun for her because she gets to revisit theories she does not currently use in her own work and has a chance to catch up on recent developments in social psychological theory. Over the summer, she teaches Crime in Global Context as part of the Liverpool Study Abroad Program, which she co-directs.
Dr. Clay-Warner says the most exciting thing about sociology is that basic sociological principles can be used to help understand so many different parts of the social world. This is what allows her to study topics that are as disparate as ‘over reward’ and ‘criminal victimization.’ In addition, because sociologists are interested in a variety of substantive topics, there are many opportunities for interdisciplinary collaboration, which allows sociologists to benefit from and contribute to other fields of study, as well as have their research reach a broader audience.
The goal of Dr. Clay-Warner’s research is to understand responses to injustice. She addresses this issue through the lenses of social psychology and criminology. As a social psychologist, she is interested in advancing basic science and engages in controlled laboratory experiments to examine how people respond cognitively, emotionally, and behaviorally when they are treated unfairly. As a criminologist, she applies this knowledge to understand the experience of criminal victimization, which she conceptualizes as an extreme form of injustice. At UGA she studies sexual violence and, more recently, human trafficking. She is also interested in understanding processes of revictimization. Specifically, she is interested in the explaining why having experienced a victimization event increases risk for a future victimization.
Currently Dr. Clay-Warner is devoted to two projects, one of which is focused on human trafficking in sub-Saharan Africa and one focused on sexual misconduct on college campuses. The first project is in collaboration with UGA researchers Dr. David Okech, Tamora Callands, and Nate Hansen, as well as researchers in the UK and in Africa. This project, funded by the U.S. Department of State Program to End Modern Slavery involves measuring the prevalence of child trafficking, as well as selecting and then evaluating prevention/intervention programs. She is particularly involved in the prevalence estimation work, which involves the application of novel sampling and statistical techniques for measuring hidden populations. The second project is in collaboration with her Sociology department colleague Justine Tinkler. They are designing a series of experiments to uncover the underlying social processes that affect men and women’s beliefs and attitudes about policies designed to counteract sexual harassment/misconduct, such as affirmative consent policies. This work builds upon Dr. Tinkler’s previous work on reactions to sexual harassment policy trainings and Dr. Clay-Warner’s work on reactions to injustice and on sexual violence.
Dr. Jody Clay-Warner joined the management team at OIBR as Associate Director in August. As Associate Director of OIBR, she oversees the faculty seed grant program, serves on the Grantsmanship Development Program Committee and the OIBR executive committee. Jody also represents OIBR in various capacities across the UGA campus and beyond.
She has been affiliated with OIBR since 2000, when she was in the Institute’s mentoring program as an assistant professor. When asked why she wanted to be the Associate Director, she said, “I know how valuable OIBR has been to me, and I want to help others benefit from the Institute. I’ve served in a number of administrative roles on campus and would like to apply the knowledge and skills I’ve acquired to advance the Institute’s mission.” Her thoughts on the future of the Institute, “OIBR’s future is bright. We are serving an increasing number of faculty across campus and are handling more grant activity than ever before. I expect this trend to continue, particularly as funding agencies become more aware of the value of interdisciplinary work.”
Dr. Clay-Warner is married to Lee Warner, who is an epidemiologist and branch chief at the Centers for Disease Control and Prevention. They met as freshmen at UNC-Chapel Hill and have been married for 27 years. Their son, Jared, is a senior at UNC-Chapel Hill, where he is double majoring in political science and communication studies. Their daughter, Avery, is a junior at UGA, double majoring in economics and criminal justice studies. That is four social science majors across two children, so clearly she did *something* right!
In her rare spare time, Dr. Clay-Warner enjoys hiking at the Botanical Gardens, pleasure reading, cooking and yoga. When asked if she had to pick another profession, what would it be? She replied, “If I were independently wealthy, I would choose to own a bookstore. I wouldn’t make any money, but I would be very happy.”
Please join us in welcoming Dr. Jody Clay-Warner to OIBR! She can be reached at (706) 542-6094 or by email: jclayw@uga.edu.

Spring 2019
RESEARCH SPOTLIGHT
Dr. Gregory Strauss (Psychology)
Interviewed by Andrea Horsman
OIBR Fellow Dr. Gregory P. Strauss, is an Assistant Professor of Psychology and Neuroscience at UGA. He directs the Clinical Affective Neuroscience Lab (CAN) and Georgia Psychiatric Risk Evaluation Program (G-PREP). Dr. Strauss received his B.S. in Psychology from UGA (2002) and PhD in clinical psychology from UNLV after completing his clinical internship at the University of Illinois-Chicago (UIC), Department of Psychiatry (2008). He then completed a two year National Institute of Mental Health (NIMH) funded postdoctoral fellowship at the Maryland Psychiatric Research Center.
Dr. Strauss’ interest in psychology and neuroscience began when he was an undergraduate at UGA. He felt very fortunate to work in the laboratory of Dr. Paula Schwanenflugel a professor of Educational Psychology, who supervised his undergraduate honors thesis and made him believe he could pursue a career in research. He was also very fortunate to have worked in the laboratory of Dr. L. Stephen Miller who helped him develop an interest in what has become his passion and the focus of his research: examining the neural basis of schizophrenia using neuroscience based methods.
He was fortunate to have some very supportive mentors in his career in Drs. Daniel Allen, Martin Harrow, Jim Gold, and Will Carpenter. They helped him to see the importance of clinically oriented research and taught him to develop skills in neuroscience that are needed to answer questions about the mechanisms underlying schizophrenia. Most importantly, they imparted a scientific philosophy of doing careful research, taking the extra time to get the details right, making his research translational in nature, and caring deeply about helping the participants in his studies. Collaborators from a number of disciplines have also been integral in allowing him to adopt new methods and theoretical approaches, which has been critical for addressing a number of scientific questions that he could not have pursued alone.
His current research primarily examines the etiology, assessment, and treatment of negative symptoms in individuals diagnosed with schizophrenia and youth at clinical high-risk for psychosis. Negative symptoms are reductions in behavior, emotion, and motivation that are common to many psychiatric and neurological disorders. There are five core negative symptom domains: avolition (reductions in the desire for and engagement in goal-directed activities), asociality (reductions in the engagement in and desire for social activity), anhedonia (reductions in the intensity and frequency of pleasurable activity), alogia (reductions in the quantity of speech), and blunted affect (reductions in the expression of emotion in face, voice, and body gestures). Once present, the five negative symptoms tend to be persistent and predict poor vocational and social outcomes, as well as low rates of recovery. Unfortunately, currently available pharmacological and psychosocial treatments have not proven efficacious for remediating negative symptoms. This is due in part to: 1) limited understanding of the mechanisms underlying negative symptoms and the fact that few clinical investigators are trained to take a cognitive or affective neuroscience approach to exploring pathophysiological mechanisms of negative symptom and 2) lack of conceptually up-to-date assessments of negative symptoms.
Much of Dr. Strauss’ work has focused on resolving these two issues. New tools were needed to enhance reliable and valid negative symptom assessment and he co-developed and validated a next-generation negative symptom rating scale for adults with schizophrenia in response to this initiative. The measure has now been translated into >20 languages and is becoming the gold-standard for use in clinical trials of negative symptoms in schizophrenia.
Dr. Strauss was recently awarded a $3 million grant from NIMH for his project entitled “Prodromal Inventory for Negative Symptoms (PINS): A Development and Validation Study.” This research will extend the measurement development efforts to youth who are at clinical high-risk for developing a psychotic disorder.
Psychotic disorders are serious and debilitating mental illnesses that incur substantial suffering for patients and present major challenges to our health care system. Given that few individuals achieve recovery after the onset of a psychotic disorder, there is increasing interest in the early identification and prevention of psychosis. Psychotic disorders are typically preceded by a prodromal (i.e., pre-illness) phase characterized by functional decline and subtle attenuated symptoms that progressively worsen over the course of several months to years. This period is of interest both as a window for investigating processes involved in disease onset and as a potential point of intervention and prevention. State of the art clinical assessments are now available to identify a group of youth at “clinical high risk” (CHR) for developing a psychotic disorder based on attenuated positive symptom criteria. However, more than 75% of youth identified as CHR do not convert to full psychotic illness within two years and currently available risk prediction algorithms are thus not optimized for sensitivity and specificity. This application takes a novel approach to enhancing psychosis risk prediction by investigating negative symptoms. In the prodromal phase, negative symptoms (e.g., anhedonia, avolition, asociality) are highly prevalent (e.g., occurring in 82% of cases) and one of the earliest indicators of risk, typically appearing years before the emergence of attenuated positive symptoms. They are often the reason why CHR youth and their families seek initial contact with the treatment system, and one of the strongest predictors of conversion to psychosis. However, currently available risk calculators do not take negative symptoms into account. This study is a three site investigation, led by Dr. Strauss, which collects data at UGA, Northwestern University (Dr. Vijay Mittal), and Emory University (Dr. Elaine Walker). Several novel risk identification methods will be evaluated, including digital phenotyping (i.e., collecting data passively via the internal sensors of the phone such as geolocation, accelerometry, and speech), social media data, and a new negative symptom clinical rating scale. The goal is to derive a new set of risk prediction measures and algorithms that can detect risk for developing schizophrenia with a high degree of sensitivity and specificity. Dr. Strauss’ hope is that these measures can be widely available for use by the general public and clinicians to enhance the detection of psychosis, leading to an enhanced ability to prevent illness onset.
Since starting his work approximately 10 years ago, Dr. Strauss has been continually surprised by the need for mental health services throughout our country, as well as the pervasive lack of knowledge about the psychosis prodrome among mental health and educational professionals. Approximately 15% of the world’s population has occasional psychotic like experiences. Often these are transitory and do not cause distress, but occasionally they warrant clinical attention. The medical and educational fields have not focused on screening for these forms of mental illness, like they have others such as autism, ADHD, or suicidal ideation. Dr. Strauss feels that screening is necessary to enhance prevention efforts, and his hope is that his research is an important step in this direction. He adds that additional efforts are needed to disseminate this information to clinicians and educators who see young people on a daily basis and can help them to receive early monitoring and intervention services that could prevent the onset of psychotic disorders.
Dr. Strauss thinks turning neuroscience-based research results into clinically meaningful products is the biggest challenge facing his field. “We have been able to develop eloquent mathematical and neuroscience models of psychiatric symptoms in our research. But, translating these models to assessments and treatments that clinicians can meaningfully use is an important challenge. Our new R01 is a step in this direction,” he stated.
Helping young people at risk for developing psychosis and becoming part of their clinical care team has been highly rewarding for Dr. Strauss and the team of graduate students and employees that he supervises. “If we can help with the process of early identification, monitoring, and prevention for even a small number of people at risk for developing a psychotic disorder, we will have made a meaningful impact on the lives of people at a time when they need it most.”
“Our research relies on rapid translation of research done in basic neuroscience (i.e., animal models) to humans. This requires a team-based approach to science, and collaborators with expertise in multiple methods. Thus, my approach to science is one that is team-based and I strive to collaborate with others who have expertise in methods and conceptual frameworks that extend my own expertise, to allow more complex questions to be answered. This has included collaborating with other psychologists, neuroscientists, computer scientists, mathematicians, and engineers,” said Dr. Strauss.
In addition to the newly funded NIMH grant, Dr. Strauss has several other ongoing grants that focus on negative symptoms.
In an ongoing R21 from NIMH (R21 MH112925), Dr. Strauss is exploring mechanisms underlying anhedonia in adults with schizophrenia using novel mathematical approaches. This study uses the ecological momentary assessment method, which involves obtaining self-reports of emotion, symptoms, context etc., as well as ambulatory psychophysiology, in the context of everyday life. This data is submitted to computational models (e.g., network analysis, Markov chain analysis, Machine Learning) that evaluate whether anhedonia reflects an abnormality in the temporal dynamics of positive emotion (e.g., the trajectory leading up to or following a planned pleasurable activity). Results have potential to lead to an updated perspective on the nature of anhedonia, as well as its underlying mechanisms. This information will be useful for developing novel psychosocial treatments of negative symptoms that utilize cognitive therapy approaches to normalize the temporal dynamics of emotion in the context of everyday life using mobile cellular phone based interventions.
In a NARSAD Young Investigator grant funded by the Brain & Behavior Research Foundation, Dr. Strauss is exploring pathophysiological mechanisms underlying negative symptoms in youth at clinical high risk for a psychotic disorder. The study aims to determine whether abnormalities in cortico-striatal function lead to disruptions in a range of reward processes that contribute to avolition and anhedonia. Studies by Dr. Strauss and collaborators have found support for such a model in adults with schizophrenia, and this will reflect the first attempt to determine whether the model extends to youth at clinical high risk for schizophrenia. To evaluate this model, a range of behavioral, EEG, and computational modeling approaches will be used in a 2 year longitudinal study of youth at clinical high-risk for psychosis. Results have potential to inform new pharmacological targets for drug development by identifying neural mechanisms underlying negative symptoms in the prodromal period.
Over the next five years Dr. Strauss said his research will continue to explore novel mechanisms underlying negative symptoms in those diagnosed with schizophrenia and youth at clinical high-risk for developing psychosis. They have recently started adopting fMRI as a new method and plan to conduct a series of studies where they examine neural mechanisms that lead at-risk youth to develop a psychotic disorder versus other psychiatric diagnoses, such as mood and anxiety disorders.
The ultimate aim of Dr. Strauss’ research is to translate results obtained in the laboratory into enhanced risk monitoring and novel treatments of negative symptoms. Focusing on negative symptoms in the prodromal phase may reflect a novel means of tracking illness progression and even preventing the onset of psychotic disorders, which are the leading medical cause of functional disability in the United States.
If you would like to read more about Dr. Strauss and his research, you can go to his lab website found here: https://ugacanlab.com/.

Fall 2018
RESEARCH SPOTLIGHT
Dr. Katherine Ehrlich (Psychology)
Interviewed by Andrea Horsman
OIBR Fellow Katherine Ehrlich, Assistant Professor with joint appointments in the Department of Psychology and the Center for Family Research, has been a very busy lady. This junior faculty member has recently been awarded three grants totaling close to $2.5 million dollars! All three research projects focus on how children’s social experiences shape their mental and physical health.
Dr. Ehrlich received her B.A. at Washington & Lee University, her Ph.D. in Psychology at the University of Maryland, and she completed a postdoctoral fellowship at Northwestern University. Dr. Ehrlich’s research, which lies at the intersection of developmental, clinical, and health psychology, focuses on how social experiences, such as early adversity, close relationships, and socioeconomic status are associated with physical health across the lifespan. In addition to utilizing a variety of methods to evaluate social and emotional functioning, her research incorporates a number of health assessments, including clinical health outcomes, measures of cellular function, and adaptive immunity. Dr. Ehrlich is a recipient of pre- and post-doctoral Ruth L. Kirschstein National Research Service Awards, a NARSAD Young Investigator Grant, an R03 from the National Institute of Child Health and Human Development, and was named a Rising Star by the Association for Psychological Science.
Dr. Ehrlich received $150,542 funding for her NIH R03 (NICHD) proposal entitled “Parental Depression and the Early Origins of Disease Across Three Generations.” When Katie joined UGA in 2016, she began working closely with Dr. Gene Brody (HDFS) and colleagues at the Center for Family Research (CFR) where she got involved in the ongoing longitudinal study of African American families (SHAPE). Youth who joined the study at age 11 are now young adults, and many of them have children of their own.
As part of this grant, Dr. Ehrlich will examine how fluctuations in parents’ (G1) depressive symptoms across a 10-year period are associated with children’s (G2) depressive symptoms and pre-disease risk factors when they reach young adulthood. In addition, they will conduct a pilot study of 60 (G3) children to evaluate links between (G1) and (G2) functioning in relation to (G3) youths’ psychosocial, behavioral, and health measures. This project will set the foundation for recruiting a third generation to the sample, which will then be extended to future projects and will allow them to address questions about the intergenerational transmission of health disparities.
Beginning in January 2019, Dr. Ehrlich will begin work on her Brain & Behavior Research Foundation (NARSAD Young Investigator) grant entitled “Skin Deep Resilience, Proinflammatory Phenotypes, and Depression Risk in Youth” with her postdoc mentors and collaborators Dr. Greg Miller and Dr. Edith Chen with Northwestern University. Also part of the project team is Dr. Gene Brody (HDFS) and Dr. Steve Beach (Psychology). The team has identified an intriguing and initially counterintuitive phenomenon. When studying resilient young adults in longitudinal samples – the participants who, despite adversity, avoided drugs, went to college, and showed few depressive symptoms – were surprisingly not resilient when it came to assessments of their physical health. In fact, these individuals fared worse than their peers, which suggested that the self-control and perseverance it required to “make it” in society was taking a toll on their health.
This research grant is important because studies of “skin deep resilience” have primarily focused on young adults. This project will recruit children (ages 8-14 years old) to examine whether these processes are evident as early as childhood. This developmental question is of particular importance because it will help to establish a time course for when diverging patterns of risk and resilience start to develop. Further, little is known about the underlying physiology that might explain why these resilient individuals develop such poor physical health in adulthood. As part of this study, they will evaluate children’s proinflammatory phenotypes by testing how aggressively their cells respond to bacteria. One hypothesis is that high levels of self-control, while protective for outcomes like academic performance and behavior in the classroom, might be associated with a more aggressive inflammatory response.
Dr. Ehrlich was also recently awarded the NIH Director’s New Innovator Award in the amount of $2,222,879 for her project “Innovative Approaches to the Study of Social Determinants of Health in Children.”
The NIH Director’s New Innovator Award, established in 2007, supports highly innovative research from promising Early Stage Investigators (defined as those within 10 years of completing their terminal research degree or postgraduate clinical training and who have not yet received substantial NIH support). This award is part of the Common Fund’s High-Risk, High-Reward Research program, which was created to accelerate the pace of biomedical discoveries by supporting exceptionally creative scientists with highly innovative research. The program seeks to identify scientists with high-impact ideas that may be risky or at a stage too early to fare well in the traditional peer review process. The program encourages creative, outside-the-box thinkers to pursue exciting and innovative ideas in any area of biomedical research relevant to the NIH mission.
This project began in 2017 when Dr. Ehrlich participated in an UGA Presidential Seed Grant challenge that encourages interdisciplinary research on campus. She submitted an application to study how stressful life experiences might dampen children’s antibody production following influenza vaccination. It was a collaborative project with Dr. Ted Ross, Director of the Center for Vaccines and Immunology at UGA. That project was not funded, but the process of putting together the application solidified Katie’s interest in using vaccinations as a way to evaluate how stress might influence children’s immune systems.
Later that year, Katie applied for the NIH New Innovator Award with the same general focus. The grant mechanism appealed to her for a couple reasons. First, the application was unlike other traditional R01 proposals – instead of a tightly focused and clear plan with preliminary data that is submitted for an R01, the New Innovator Award asks you to think about a scientific challenge that you want to address and how you might take a novel approach to solving that problem. No preliminary data are required, nor do they require the specification of a clear experimental plan (and NIH discourages applicants from submitting specific aims).
The New Innovator Award research is important because the examination of links between social stressors and physical health is difficult to do in childhood, in part because children are generally healthy and show few signs of outward disease. This research will allow them to circumvent some of the challenges they’ve previously faced when trying to examine health markers that have little variability or prognostic utility in childhood. They will be looking at children’s response to vaccination as an indicator of physical health – a measure that can be considered an in vivo marker of immune function with clinical health relevance.
The odds of success for winning the NIH New Innovator Award are low. It was determined that, out of 600 funded proposals over the last 11 years, only seven other awardees were from psychology departments. So… congratulations Dr. Ehrlich on this huge accomplishment!
Dr. Ehrlich feels that access to unique resources at UGA were a major part of her grant successes. As a participant of OIBR’s Grant Development Program, she workshopped the project idea throughout Year 1 of the program and those discussions plus the focused time to write allowed her to put forward a competitive proposal. The Clinical and Translational Research Unit (CTRU) is a phenomenal facility, with ample space for data collection (e.g., patient rooms) and the staff to help with the visits. In particular, their nursing team is invaluable for blood draws and vaccine administration. Working with vaccines and evaluating antibody production was completely new for Katie, and she was fortunate to rely on the Center for Vaccines and Immunology center (and director Ted Ross, in particular) to assist with study design, sample assays, and answering all of the questions that pop up with this research.
“In addition to being an incredibly kind and supportive mentor, Dr. Gene Brody (HDFS) has encouraged me so much along the way. Also, the collaborative and supportive nature at CFR has far surpassed my expectations for what it would be like to work at UGA, and as a result of CFR’s support, I have been able to move quickly on these applications. I’m confident that these proposals were funded at least in part because of the support and infrastructure that CFR provides for assisting with research,” said Dr. Ehrlich.
So what are the long term goals for this young investigator? Dr. Ehrlich is interested in how these processes play out over time, both within individuals and across generations. She and Dr. Brody are planning to expand on the R03 project to recruit all of the G3 children in the study so that they can more fully examine how experiences in one generation carry forward to the next. She is also interested in new techniques that will provide better insight into the biological mechanisms that might help explain, in part, how social experiences come to influence health.
When asked what she finds most rewarding about her research, Katie replied, “It’s hard to pick just one part! I love how interdisciplinary and collaborative my work is. There’s always something new to learn and a new potential collaboration on the horizon. I’m also really excited about how our work has the potential to inform interventions and public policy – for me, it brings deeper meaning and more urgency to our work.”
To get updates about the progress on all of these projects, please visit Dr. Katie Ehrlich’s lab The Health and Development Laboratory here.


SPRING 2018
RESEARCH SPOTLIGHT
Dr. Denise Lewis (HDFS)
Interviewed by Andrea Horsman
OIBR Affiliate Denise Lewis, Associate Professor in Human Development and Family Science, was awarded a $3+ million grant from National Academies of Sciences, Engineering, and Medicine for her project entitled “Community and Family Resilience, Strength and Well-being: Sociocultural Influences on Cambodian and Laotian Refugee Communities’ Responses to Environmental Challenges.” We recently caught up with Denise and asked her to share some information about her project.
How did you first get involved with this project?
I read the request for proposals in October 2016 and began crafting ideas for the project. I knew I’d need a strong team so I traveled to the Alabama coast to meet with leaders in the Cambodian and Laotian communities (where I have more than 20 years of research history). I initially worked with my long-time collaborator, Dr. Desiree Seponski (HDFS) and four community partners. As ideas evolved, I added faculty from the College of Public health: Dr. Sarah DeYoung aids in community psychology research, and there is a disaster preparedness assessment and training component as well.
Tell me about this project and why it is important-
Southeast Asian refugee families living along coastal Alabama have endured cumulative effects of multiple traumas. These include Cambodian refugees’ flight during the Pol Pot genocide that led to approximately two million deaths and an exodus from Laos and Vietnam at the end of the United States-Vietnam War. Families from those nations witnessed deaths of loved ones and continue to experience separations caused by resettlement and adjustment to life as immigrants/refugees. Many families resettled in the United States (US) found that local populations were far from welcoming. Members of the Alabama coastal community faced hostility as they began work in the seafood industry. More recent traumas include the massive destruction caused by Hurricane Katrina and the Deepwater Horizon oil spill. These traumatic experiences can create long-felt social pain and mental anguish, but can also serve as mobilizers for community resilience. It is this foundation of individual, family, and community resilience from multiple traumas that this project will explore.
This project will contribute to three main sociocultural objectives of human dynamics tightly linked to resilience: (1) Engagement of the refugee community through collaboration on, development, testing, and implementation of empirically-informed, community-driven, and community-based programs that produce immediately usable information to prepare for, adapt to, and mitigate effects of environmental challenges; (2) Training community members in research, grant writing, and hazardous risk management skills to facilitate sustainability of developed programs/processes; (3) Creation of models of community-based risk reduction and household production of health including individual, family, and community intersections of sociocultural factors associated with strengths and vulnerabilities.
Tell me about someone who has influenced your decision to work with these communities-
More than 20 years ago, I volunteered to teach English to a Cambodian monk who had just arrived in the United States. One of the community leaders, Mr. Heang Bun Chhun, organized a group of older couples to teach me about Cambodia and Cambodian life- ways as I was teaching the monk. Mr. Chhun’s strength, his willingness to teach and tell his and other refugees’ stories, and his dedication to advancing the good of his community have strongly influenced my decision to continue my work with this and other refugee communities. Through him, I’ve learned that even the most outwardly disadvantaged people possess an inner strength that can be brought to bear on nearly overwhelming circumstances. Refugees, such as those I work with in Alabama, arrived in the US with no material possessions, very limited to no English language skills, and were filled with grief over the loss of many, many family members and their homes, inspire me through their strength and resilience.
What has surprised you most about working on this project?
The most surprising aspect of this project is the willingness of so many members of these two refugee communities to work together, with me and others, to build a stronger community of identity. It is obvious to me that they want to see their cultures survive and thrive. They want to be sure they are providing a foundation for future generations who are proud of their heritage.
What do you find most challenging about this research project?
The greatest challenge is working across three different languages. Although an individual may speak one or more languages, they may not be literate in any of them. Fortunately, I have four main community partners (2 Cambodian and 2 Laotian) who are all fluent in their native language and in English. I also have four translators/transcribers who assist and an additional 20+ members of a cultural advisory board. Without individuals such as these working with me, it would be extremely difficulty to accomplish the goals of this project.
Tell me about some of the people you’ve met-
I’ve known Mr. Heang Bun Chhun for more than 20 years. He escaped from Cambodian in 1976 after losing most of his family. In the early 1980s, he and two other Cambodian refugee men purchased about 180 acres of forestland and created a Cambodian village. He has been my chief Cambodian collaborator since 1996 and is now a close friend. Samoeuy Chim is another Cambodian collaborator. She arrived in the US as a child and has become a very successful businesswoman—she owns several service stations and a chain of doughnut shops. She is constantly “giving back” to members of the local refugee community. Her quiet generosity is inspiring. I’ve known her for more than 20 years as well. I am well known in the Cambodian community—a factor that made creating and now implementing this project a reality.
It has been a pleasure to begin to know members of the Laotian community. The two communities tend to interact so, over the years, I had met many Laotian refugees. However, it wasn’t until Mr. Chhun organized a community meeting in 2016 with leaders from both the Cambodian and Laotian communities that I really began to know Laotian refugees. The primary Lao leader is Mr. Vi- sanou Khamphouy. He arrived from Laos about 40 years ago and is the head of a very large Laotian family. He also engages in mul- tiple community-building activities. These three individuals (Chhun, Chim, & Khamphouy) are collaborators on the grant. There is a fourth individual, Khiaw Srihanouvong, who volunteers his time in the community and in service to the goals of the project. Mr.
Srihanouvong is highly engaged in outreach and in organizing volunteers to serve the communities. He has become a vital part of the project. All of these individuals display strong commitments to their communities and to the project and provide input into how to best meet the needs of their communities.
What is your personal philosophy on what should be done about refugee and immigrant communities?
We should talk to refugee communities about what they see as their greatest need and provide opportunities that respond to those needs. We must recognize the strengths and resilience within these groups. It is vital that we embrace their knowledge, walk with them as partners and, eventually, move out of the way so they can build communities in such a way that they are able to thrive instead of remain in a state of marginality and dependency.
What do you think will change over the next five years?
These communities will thrive by engaging in culturally relevant community building. I already see (and hear) plans for teaching children the languages and traditional dances. Community members are excited about the upcoming community grant writing course (happening in May) and how they’ll work together on issues they have identified in their communities as needing additional funds to address.
What else can you tell me about this research?
This research-practice project has the potential of making generations-long changes to benefit these two Southeast Asian refugee communities.
What benefits (if any) have you experienced by working with OIBR on this grant?
The greatest benefit I’ve received from OIBR on this grant is that I have a team of experienced and knowledgeable people who’ve worked with me from the very beginning to address all the requirements of the funding agencies, to help me think through the needs of the project, and to assist with hiring, budgeting, and managing the grant so that I can focus on the science and implementation of the project.
Where can people go if they want to learn more about this project?
People can learn more by visiting our website http://www.fcs.uga.edu/hdfs/clcsrp or our Facebook page @CamLaoStrong.
